(The Center Square) Several major health insurance companies are vowing to make changes to simplify their prior authorization process and improve Americans’ access to timely health care.
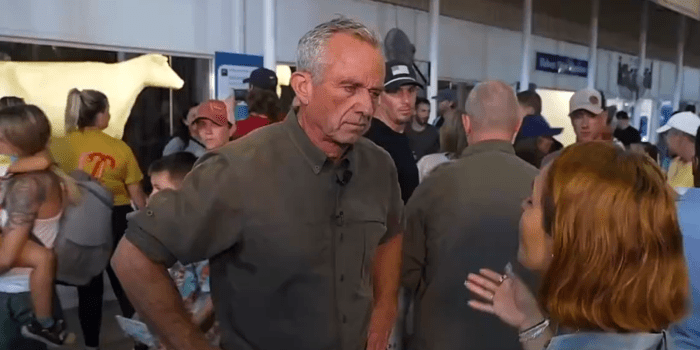
U.S. Health and Human Services Secretary Robert F. Kennedy Jr. and Medicare & Medicaid Administrator Dr. Mehmet Oz announced the changes during a news conference Monday afternoon.
“Patients should not be waiting because bureaucratic hurdles are blocking their medical treatment,” Oz said Monday.
Oz and Kennedy announced plans to collaborate with numerous health-care insurers, including UnitedHealthcare, Blue Cross Blue Shield and Kaiser Permanente, to implement grace periods when patients change plans and utilize electronic systems to speed up prior authorization.
“Americans shouldn’t have to negotiate with their insurer to get the care they need,” Kennedy said. “Pitting patients and their doctors against massive companies was not good for anyone.”
These commitments made by health insurance companies were not prompted by federal mandates from HHS or CMS but were rather made on a voluntary basis.
“We applaud these voluntary actions by the private sector, which is how these types of issues should be solved,” Oz said. “CMS will be evaluating progress and driving accountability toward our shared goals as we continue to champion solutions that put patients first.”
Healthcare trade association America’s Health Insurance Plans (AHIP) announced that insurance companies are seeking to launch standardized electronic systems for prior authorization by Jan. 1, 2027.
Insurers are also aiming to decrease the number of health-care claims that require prior authorization screening by Jan. 1, 2026.
“These measurable commitments – addressing improvements like timeliness, scope and streamlining – mark a meaningful step forward in our work together to create a better system of health,” Blue Cross Blue Shield CEO Kim Keck said.
Read full article here