Even on mornings when I’m in a rush to get somewhere on time or nights when I can hardly keep my eyes open, I never skip brushing my teeth. And it’s not just because I want to avoid cavities, crowns and root canals.
I’ve read article after article talking about the connection between the health of my mouth and the health of other parts of my body. As weird as it may seem, fending off gum disease can have a direct impact on your heart, lungs and brain — and that’s just the start.
Now it looks like we can add another organ to that ever-growing list…
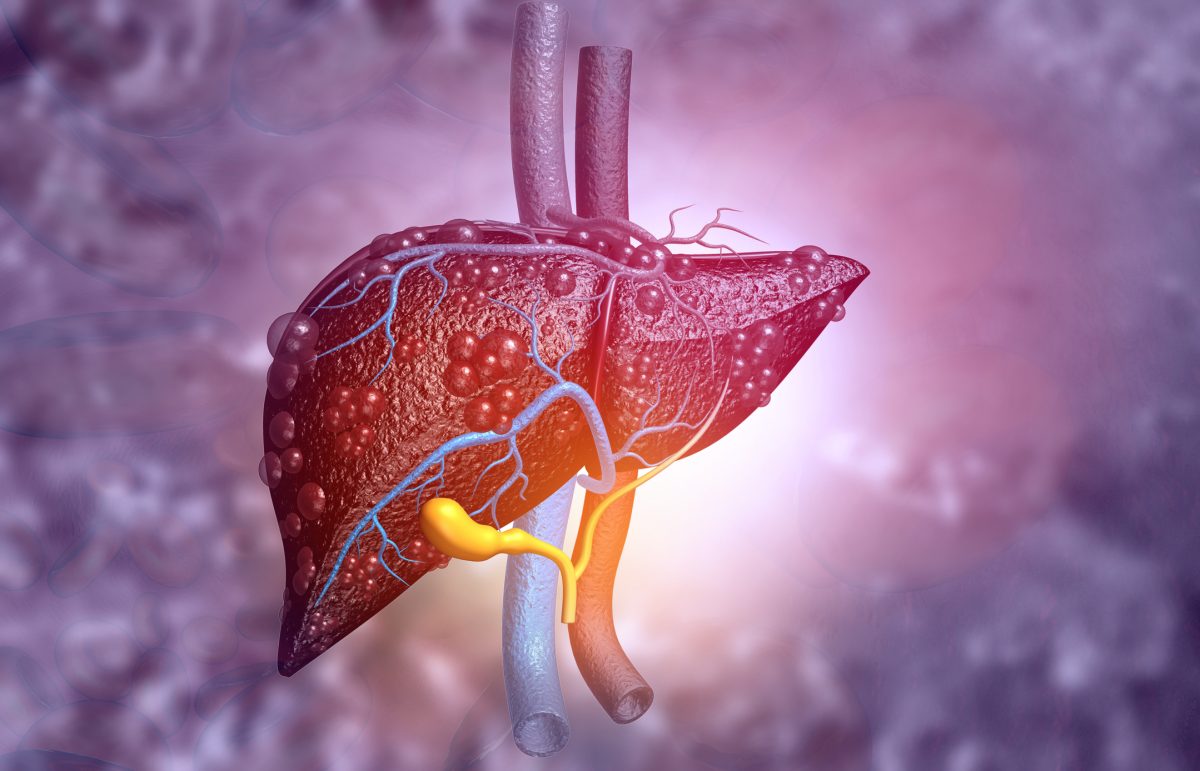
The road from your mouth to your liver
Gum disease, also known as periodontitis, is a widespread chronic inflammatory condition caused by bacterial infections in the gum tissue of the mouth. Its severity tends to increase with age, smoking, alcohol use and poor dental care.
Not only can it wreck your dental health, leading to bleeding gums, bad breath and tooth loss — but it’s also linked to several other severe conditions, like heart disease, diabetes, dementia and maybe even cancer.
People with liver disease are already at higher risk for these dangerous conditions. So, for them, getting gum disease compounds those threats. But it gets worse…
An international team of researchers discovered multiple ways that periodontitis may directly aggravate liver disease — starting with the “oral-gut-liver axis”…
The bacteria that cause periodontitis can be swallowed or enter the bloodstream during activities like chewing or brushing and make their way to the gut. Once there, they can cause dysbiosis, an imbalance between good and bad microbes, and leaky gut, a condition that makes the gut lining permeable. Endotoxins — byproducts produced by bacteria — can then easily make their way to the liver, triggering inflammation and causing the type of damage that leads to liver fibrosis.
Previous studies have shown that bacteria such as the one that causes gingivitis can exacerbate inflammation and a buildup of fat in the livers of mice with pre-existing metabolic diseases. These microbes or their byproducts have even been found in liver tissue, suggesting that movement from the mouth to the liver is not uncommon.
Next, the immune system gets involved: Chronic periodontal inflammation leads to the release of pro-inflammatory cytokines, such as TNF-alpha and IL-6, which have been long associated with the progression of liver disease. In addition, the review highlights Th17 cells, a type of immune cell activated by oral pathogens that may travel to the liver and worsen metabolic dysfunction.
The bottom line: These pathways form a terrible merry-go-round of liver disease-impairing oral health and inflammation that drives liver damage.
Human studies reinforce the connection
Data from human studies support this association. Patients with cirrhosis consistently demonstrate worse oral health than the general population, with higher rates of gingival overgrowth, tooth loss and bone loss. In fact, the prevalence of periodontitis among patients awaiting liver transplants can be as high as 72 percent!
Other studies have found links between severe periodontal disease and increased death risk in cirrhosis patients — and that people with advanced periodontitis are much more likely to have metabolic dysfunction-associated steatotic liver disease (MASLD), the most common form of chronic liver disease. This was true even after adjusting for risk factors like obesity and diabetes.
One small trial showed that periodontal treatment led to a short-term improvement in liver enzyme levels, indicating that oral health interventions may influence liver function.
The review authors caution that this research is still in the early days. However, the review calls for better collaboration between specialists who manage liver disease and dental professionals who manage oral healthcare.
In the meantime, it’s clear that oral hygiene is paramount, especially for those with chronic liver conditions, as well as twice-yearly dental visits. Take note of any changes to alert your dentist to — like persistent bad breath and red, swollen, tender or bleeding gums.
A dental probiotic can boost the oral microbiome. You’ll want the dental probiotic to be in a form that allows it to stay in the mouth for enough time to be absorbed by the microbiome. Some good delivery forms are lozenges, drinks, mouth rinses or chewable tablets.
If you have liver trouble, ask your doctor about supplements. Omega-3s have been shown to support liver health and guard against gum disease.
Sources:
Bad breath, bad news: how gum disease could worsen liver conditions — EurekAlert!
Periodontal disease and cirrhosis: current concepts and future prospects — eGastroenterology
Read full article here